Request accessible format of this publication.
Grenfell MPS clinical services plan 2020-2030

About Grenfull Health Service
Grenfell MPS is a rural facility within Western NSW Local Health District (LHD). It provides a range of inpatient, outpatient and community clinical services to Grenfell and surrounding communities, and works as part of a network of health services and hospitals within the region.
The Plan has been developed for Grenfell MPS. It describes the key directions for Grenfell MPS over the next 10 years to support healthier lives for people living in Grenfell and local surrounding communities, and deliver reliable and contemporary health care both inside and outside of the MPS setting.
Why we need a plan
Grenfell MPS is the primary provider of hospital services to the people of Grenfell and surrounding communities. The Grenfell population is predicted to decline over the next 10 years, and like other parts of Australia the population is ageing.
There are higher rates of chronic disease, and inequalities in the health and wellbeing between some groups in the community which are important challenges for the future.
The Plan has been developed to respond to these challenges by considering the health needs of the population, services to meet these needs and the infrastructure requirements for Grenfell into the future.
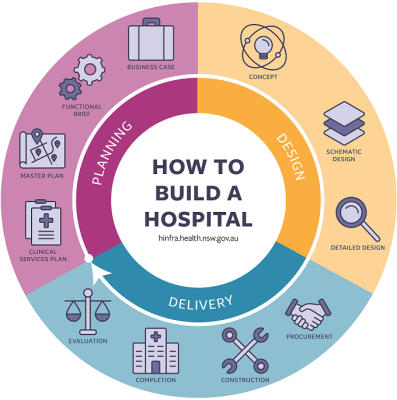
A CSP is the first step for any significant facility refurbishment or redevelopment. NSW Health Infrastructure's - How to Build a Hospital (pictured) outlines the steps in the process.
Grenfell MPS catchment
The Grenfell MPS provides services to the local community, across the Weddin Local Government Area (LGA). The Weddin LGA also includes the villages of Caragabal, Quandialla, Greenethorpe and Bimbi.
The total estimated population of the Weddin LGA is approximately 3,677 persons. According to the NSW Department of Planning, Industry and Environment (2019), it is anticipated that in 2031, the population of the Grenfell MPS catchment area will decrease by 14% to 3,172 persons.
Population projections suggest continued growth in the 70 years and older group to 28% of total Weddin population in 2031. This is consistent with the ageing population across NSW.
Grenfell MPS catchment: Health needs
People living in Weddin LGA were more likely to experience a chronic condition than the rest of NSW. The most common chronic conditions seen are diabetes, vascular disease, respiratory disease, and mental health.
Weddin residents have some health indicators comparatively better than the rest of the Western NSW LHD area, and NSW population. These include:
- life expectancy, which is higher compared to the rest of NSW and the LHD
- lower rates of high blood pressure
- high psychological stress
- cancer deaths
- alcohol-attributed hospitalisation.
However, Weddin residents experience higher than NSW rates of:
- cardiovascular disease hospitalisation and deaths
- diabetes hospitalisations and deaths
- hospitalisations due to injury and poisoning
- mental health hospitalisations
- mothers smoking in pregnancy.
Behavioural and modifiable risk factors include:
- smoking
- alcohol consumption
- inadequate fruit consumption
- inadequate physical exercise.
These behavioural risk factors have been associated with the development of chronic disease.
Health related behaviours for the Weddin population (compared with the rest of NSW) include:
- smoking Rates (smoking in the general population and smoking in pregnancy) are greater than the rest of NSW
- lower exercise, as defined as 30 mins of moderate activity on most days of the week
- higher rates of alcohol consumption (>2 alcoholic drinks per day)
- higher proportion of the population who are obese
- higher proportion of people who have one or more behavioural risk factors.
Community consultation
Consultation has informed the development of the Plan, and has included:
- engagement with Grenfell Health Advisory Council
- consultation workshops with 3 stakeholder groups
- engagement with the Weddin Shire Council
- local and LHD specialist staff consultation initially and then on key draft plans.
The key health needs and issues identified by the community included:
- mental health services
- transport systems and services
- issues with the current infrastructure and functionality of the Emergency Department supports for an ageing population
- palliative care
- telehealth
- connection to local history, community and Indigenous culture
- hospital infrastructure and services
- partnerships
- workforce
- medical imaging
- access to transport.
Current services
Grenfell MPS provides residential aged care, acute and subacute care include palliative and respite care, and a range of primary and community health services.
Drivers for change
There are a number of factors driving change in health care for the Grenfell community. These include:
- Age and function of the current infrastructure of the health service.
- The changing profile of the population, with an increase in the number of people aged over 70.
- The prevalence of chronic diseases and risky health related behaviours.
- Workforce.
- Changing models of service delivery and new and emerging evidence, including:
- virtual health
- alternatives to in-hospital care
- enhanced and integrated primary care
- shorter length of stay and proactive community following.
- Geography.
- Community expectation.
By reviewing the historical activity for Grenfell MPS, understanding the health needs for the Cowra region, the projected changes in the population, and listening to the community, we develop the Clinical Services Plan.
The way forward
The draft Plan describes a vision for Grenfell MPS over the next 10 years, including its role in a network with Cowra, and in delivering urgent care, inpatient acute and subacute care, residential aged care, and community based care.
The Plan responds to the needs of the community, and outlines the opportunity for an integrated and digitally connected health and wellbeing approach to healthcare, alongside contemporary acute care. The key directions for Grenfell MPS include:
Improved health and wellbeing of rural people
- Improved management of people with chronic conditions and complex health needs through an emphasis on prevention, health promotion and risk reduction, early intervention, rehabilitation and self-management strategies.
- Improved mental health service provision (particularly for young people), with outreach follow-up in the community.
- Expansion of the current ambulatory care and hospital in the home services.
- Health promotion activities focused on mental health and drugs and alcohol use in young people,
- Increased usage of telehealth to engage with consultants and to provide education/training opportunities for both staff and the community
- An increased focus on the ‘first 2,000 days’ in partnership with local general practitioners, local schools and other health and health related services.
Meaningful gains in Aboriginal Health
- Working in collaboration with key stakeholders to achieve meaningful gains in Aboriginal health. This will include strong advocacy for flexible services that facilitate access, participation and an appreciation and acknowledgment that ‘making a difference’ requires innovation, flexibility and new ways of doing business.
- Improved service provision to Aboriginal and/or Torres Strait Islander people through ongoing consultation, involvement in care planning and the implementation of culturally appropriate service delivery models.
- Increasing the percentage of Aboriginal peoples working at Grenfell MPS particularly in front line positions.
- Physical infrastructure should consider features that make Aboriginal peoples feel respected and safe and reflect cultural needs and practices.
World class rural health care
- Inpatient care that aims to prevent, reverse, stabilise or slow functional decline and models of care that focus on an enabling approach, building capacity in independence, empowerment and autonomy.
- Workforce planning to ensure Grenfell MPS is appropriately resourced to achieve high quality inpatient and community based, and integrated chronic care.
- Working with NSW Ambulance to develop safe and sustainable models of emergency care and alternate care pathways (particularly for chronic conditions and end-of-life care) that benefit the community, reduce emergency department presentations and avoid hospital admissions.
- Ensuring health/aged care workers are appropriately trained, qualified and possess the necessary knowledge and skills to deliver high quality, evidenced-based, compassionate chronic and complex aged care to meet the needs of our ageing population.
- Expansion and upgrades that support contemporary acute care, integrated chronic care, and residential aged care best practice service models.
One health service across many places
- Partnering with general practitioners and the NSW Ambulance service to increase uptake of advanced care directives and end of life care planning.
- Working in partnership with other care providers including NSW Ambulance Services, residential aged care services and non-government health related providers to reduce unnecessary hospital admissions, provide acute and post-acute care services in residential aged care facilities, and supporting people to remain in their communities.
- Exploring the opportunities to use virtual to provide greater access to specialist services.
- Developing collaborative partnerships with aged care providers, non-government agencies, primary health care providers and general practitioners to enhance palliative care services in the community.
- Develop strategies in partnership with specialist palliative care services to increase timely access to specialist consultants and support services for both patients and generalist clinicians.
The Plan includes infrastructure needs to future proof Grenfell MPS including an increase in residential aged care beds, and improve access to care using a network of services in the region.
Next steps
The Grenfell MPS Clinical Services Plan is now with the Ministry of Health for final review and endorsement.