Request accessible format of this publication.
Bathurst Clinical Services Plan 2022-2031

About Bathurst Health Service
Bathurst is one of the largest population centres in the Western NSW Local Health District and the Bathurst Health Service plays an important part in providing care to the local community, and as part of a network of healthcare services in the region.
Bathurst Health Service includes Bathurst Hospital, which is a major referral hospital (‘Base Hospital’) that delivers a range of inpatient, outpatient and community clinical services. Bathurst Health Service is the primary provider of hospital services to the people of Bathurst and surrounding communities.
Who uses the Bathurst Health Service
Bathurst Health Service provides services to the local community of Bathurst and the surrounding communities of Oberon, Blayney, and parts of the Mid-Western Local Government Area (LGA). People from Lithgow LGA also access services at Bathurst.
The total estimated population of the Bathurst Health Service catchment area is approximately 56,300 people (2021 Census). According to the NSW Department of Planning, Industry and Environment (2022), it is anticipated that in 2036, the population of the Bathurst Health Service catchment area will be around 66,000 persons.
Most of the population change is in the Bathurst Regional LGA (53,710 people in 2036) and the older age groups, however the number of children aged 0-14 years is also projected to increase.
Find out more about Bathurst Health Service
What a clinical services plan is
The first stage in the redevelopment of a hospital is clinical services planning. The Bathurst Community and Region Integrated Clinical Services Plan (CSP) 2022-2031 outlines the health services requirements for Bathurst Health Service over the next 10 years.
The CSP was developed in 2019-2020 and then updated in May 2022. The CSP was re-submitted for review in mid-2022 and was endorsed by the NSW Ministry of Health in early 2023.
Why is a CSP important?
The CSP considers how the health needs of the community can be met into the future and looks at some of the things that change both the population and the needs of a population such as:
- How a community is growing and ageing - In Bathurst, regional migration drive appears to be speeding up population growth and this may also change the makeup of the population. For instance, it may lead to more younger adults, families and children in the region.
- Health conditions - People in the Bathurst region have higher rates of chronic disease than the state average. The most common chronic conditions seen are diabetes, vascular disease, cancer, respiratory disease and mental health conditions.
- Behaviour - People in the Bathurst region have higher rates of behaviour that can lead to poorer health, including obesity, smoking, alcohol consumption and inadequate exercise.
- Population profile - There are poorer health outcomes in some population groups in the Bathurst region, including Aboriginal peoples.
- Service demand - Changes in the age and health needs of the community, as well as changes in how healthcare is provided is growing demand for health care services in the Bathurst region.
- Models of care - Healthcare is always evolving to improve outcomes, quality, experience and access. Looking how changes such as virtual healthcare, better primary care, shorter hospital stays, better integration and collaboration across services, and improving out-of-hospital care is a feature of the CSP.
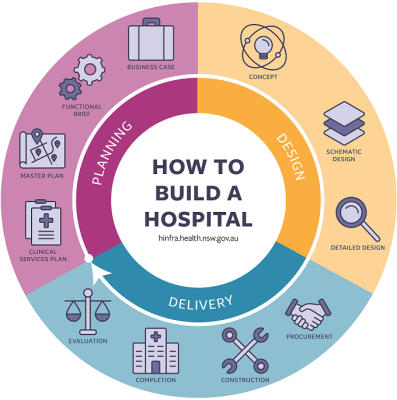
NSW Health Infrastructure's - How to Build a Hospital (pictured) outlines the steps in the process.
How the plan was developed
Western NSW LHD developed the CSP in consultation with health service clinicians and staff, consumers and community members, as well as service delivery partners, universities and local government.
The process included significant stakeholder consultation featuring:
- the formation and use of a CSP Steering Committee and Clinician Advisory Group
- information from 162 survey responses from staff and community members
- 18 consultation workshops involving 66 clinicians
- consultation with Bathurst Clinical Council and Bathurst Health Council
- community forums involving around 40 community members
- Aboriginal Yarning Circle
- 14 meetings with key stakeholders
- feedback from the release of the draft CSP.
What was identified
The key health needs and issues identified during consultation included:
- Reducing the need to travel by providing services locally. Services highlighted in the CSP included: emergency orthopaedics, respiratory medicine, cardiology, palliative care, psychiatry/mental health, ENT, eye surgery, urology and MRI.
- Hospital infrastructure, including overall space and functionality.
- Current and future workforce requirements.
- Improve the ‘journey’ a person experiences from the time they arrive at hospital, are admitted into a bed, all the way through to their discharge from hospital.
- Taking services to the people by growing and developing ambulatory and services provided in the home, and meet the demand for outpatient services including clinics.
- Improve access to services for Aboriginal peoples and support the Aboriginal patient journey.
- Transport systems and services, including transport back home after treatment if required.
- Embrace technology and innovation.
- Improve how people in custody are managed in the emergency department and on the wards.
- Recognise the impact that the National Disability Insurance Scheme (NDIS) is having on staff of Bathurst Health Service.
- Partnerships with other organisations, healthcare providers, patients and carers.
The way forward
The CSP responds to the health needs of the community now and in the future, and identifies priorities for Bathurst Health Service. Some initiatives outlined in the CSP are dependent on additional resources.
- Focus on services that address developmental delay, behavioural issues, child mental health and other issues found in children the Bathurst region.
- Work with our partners to develop a Child and Family Service ‘hub’ focused on the first 2000 days, and on vulnerable children.
- Reinvigorate the focus on the overall health of the population by working with local Councils and other services to help keep people well.
- Expand ambulatory, community-based and home-based services, and provide more services in people’s homes, and closer to where they live.
- Enhance community health services and consider the best location for these services to promote ease of access and wellness.
- Establish a multidisciplinary ‘Older Person’s Flying Squad’ to provide acute care to older people at home and in residential aged care.
- Embed and expand the new community rehabilitation service.
- Enhance priority medical services particularly respiratory medicine and cardiology, and expand specialist outpatient care by introducing new clinics and outpatient services including ophthalmology – potentially through a public private partnership model, ENT, respiratory, endocrinology, diabetes and neurology.
- Continue to embed the Orthopaedic Acute Surgical Unit model of care and improve functioning of the fracture clinic.
- Enhance local access to priority surgeries including eyes, ears nose and throat (ENT), scopes and planned urology.
- Enhance pre-admission services including multidisciplinary preadmission clinic.
- Adopt a whole-of-person approach to mental health and drug and alcohol service.
- Make sure patients are cared for in the right place, at the right time while they are in hospital by improving patient flow through the whole-of-hospital – from admission to discharge.
- Work with partners to improve access to care for patient after they leave hospital.
- Enhance palliative and end-of-life care services and work in partnership with General Practitioners (GPs) and other service partners including aged care facilities to improve consumer choice and quality of end-of-life care.
- Review maternity and Emergency Department models of care to improve functioning and support best-practice and high-quality patient care.
- Implement contemporary models of care in the care of medical and surgical patients.
- Enhance clinical and non-clinical support services so that they can function well, meet all relevant standards and policies, and be able to support the expanded clinical services at Bathurst Health Service.
- Enhance access of Aboriginal people to services and support the Aboriginal patient journey.
- Recognise and address the impact of the NDIS on patients and their families and clinicians, particularly a lack of other providers for assessment and therapy.
- Explore with Justice Health and Forensic Mental Health Network telehealth service options for the prison population.
- Further our virtual care / videoconferencing capability and embrace technology and innovation.
- Further develop Bathurst Health Service as a teaching, learning and research hub.
- Work with our partners on any further planning for a health, research and education precinct in Bathurst.
- Work with the Commonwealth and State Governments to introduce in-hospital Magnetic Resonance Imaging (MRI) scanning. Note that this service became operational in early 2023.
- Work towards future-proofing Bathurst Health Service, matching available bed capacity and treatment, clinic and group spaces to projected demand.
What infrastructure requirements have been identified
The existing hospital footprint needs to be changed in order to meet the current and future demands on the service.
- Expand community-based and outpatient services.
- Significantly expand the Ambulatory Care Unit.
- A revamp of outpatient treatment areas.
- Provide additional clinic/therapy rooms for specialty clinics.
- Enhance capacity of community health and consider best location to support ease-of-access.
- Increase the capacity of the Dental Clinic.
- Increase the number of chemotherapy chairs.
- Develop an outpatient, chair-based maternity service.
- Expand the Emergency Department.
- Provide additional ED treatment spaces, and establish a Behavioural Assessment Unit within the ED.
- Increase the ED Short Stay Unit.
- Improve the design and adjacencies of the unit including Fast Track zone.
- Increase inpatient beds.
- Build approximately one extra adult medical ward, with consideration of a dedicated area for coronary care patients and for Medical Assessment Unit (MAU).
- Increase the number of ICU/HDU beds and move Coronary Care out of the existing ICU/HDU area.
- Surgical bed uplift, with consideration of a 23-hour surgical Model of Care.
- Small maternity inpatient bed and Special Care Nursery expansion.
- Small rehabilitation inpatient bed expansion.
- Overhaul a number of existing ward areas to improve how patients flow through the hospital and to support staff to provide best-practice, contemporary care.
- Develop a dedicated Transit Lounge to facilitate earlier discharge from the ward.
- Enhance the Peri-Operative Suite.
- Consider 4 fully-sized operating theatres and 1 procedure room.
- Peri-operative and post-anaesthetic recovery spaces will be looked at.
- A new mental health facility is one of the options being explored to ‘unlock’ the hospital footprint – this would combine both inpatient and outpatient/community-based MHDA services into a single building.
- Provide additional consult/interview rooms for integrated MHDA community services.
- Ensure clinical support areas are right sized to match expanded bed base and outpatient services.
- Provide additional outpatient ultrasound space and consider dedicated recovery bays within Medical Imaging to support planned increase in interventional radiological procedures. Plan for future CT requirements.
- Enhance Pathology Unit to ensure sufficient capacity, optimise workflows and support its functions and range of services (with NSW Pathology).
- Enhance Pharmacy Unit to support more efficient workflow and sufficient space to support its functions.
- Enhance Sterilising Department to support additional equipment to meet future demand.
- Sufficient non-clinical services and support space / areas to support the increased bed base and footprint including staff office space/meeting rooms/amenities, and storage space.
- Enhance training centre facilities to support more students and also multidisciplinary education.
- Staff / student accommodation requirements.
Common questions
The CSP is not a blueprint for the hospital redevelopment, it is a plan that reflects the current and projected health service needs of a community at a point in time. It is one of the many sources of information that informs the future direction of a new hospital. The final size and shape of the redeveloped Bathurst Health Service will be determined in the master planning phase and next phase of design, be subject to the State Significant Development Application and informed by staff, community and consumer consultation.
Yes. The redeveloped hospital will deliver an increase in bed numbers and clinical spaces.
Where we are now – early 2023
On 15 June 2022, The Hon. Paul Toole, MP, Deputy Premier, Member for Bathurst and The Hon. Bronnie Taylor MLC, Minister for Women, Regional Health and Mental Health announced $200 Million for the redevelopment of Bathurst Health Service.
The Ministry of Health approved the CSP in early 2023.
Health Infrastructure (HI) is overseeing the Bathurst health Service Redevelopment on behalf of the NSW Government. HI manages the planning, design and delivery of all health infrastructure capital works worth over $10 million throughout NSW. There is also a dedicated project team which is composed of representatives from Western NSW Local Health District, Bathurst Health Service staff, Ministry of Health and the lead design team.
The redevelopment of Bathurst Health Service project is in the master planning phase, informed by the approved CSP. The Master Plan for the Bathurst Health Service development will deliver the clinical needs identified in the CSP. Master Planning provides a clear framework that defines and prioritises areas for the new hospital, now and into the future. The facility will be designed with the capacity to grow as demand for services changes and a building structure that supports staged expansion beyond the foreseeable demand projections.
Construction of the redevelopment is expected to be completed in 2027 with work to build the expanded health facility will be carefully staged to ensure clinical services remain operational during construction.
Planning and design of the redevelopment is a collaborative process involving consultation with clinicians, staff, patient groups, local stakeholders and the community. Opportunities for staff, community and stakeholder participation will be communicated as the redevelopment progresses.
Further information is available on the Bathurst Health Service redevelopment website.